Medical Therapies For IBD Treatment
If you have been diagnosed with IBD, there are a variety of gastrointestinal medications available that can help treat, and sometimes completely suppress, your Inflammatory Bowel Disease symptoms. Our doctors will work with you to find the medical treatment that is right for you, based on a variety of factors like your symptoms, history, and lifestyle preferences.
Inflammatory Bowel Disease is a chronic condition with a variable course. Both Crohn’s disease and Ulcerative colitis may vary in severity from mild to severe. Depending on the severity of inflammation, different medical therapies may be indicated. The same individual may start out having mild disease but over time progress to more extensive disease requiring an intensification of medical therapy. Here is a brief overview of the most commonly used gastrointestinal medications and medical therapies for IBD.
Mesalamine is an anti-inflammatory compound which has been used the longest for the treatment of Crohn’s disease and Ulcerative colitis. It comes in different preparations, including oral and rectal preparations (enemas and suppositories). The most common oral preparations are Pentasa, Asacol, Lialda and Apriso. While both, oral and rectal preparations, are effective in mild to moderate Ulcerative colitis, its efficacy in Crohn’s disease has been questioned. Therefore, Crohn’s disease patients with significant inflammation may require stronger anti-inflammatory and immune suppressive medications.
Steroids, such as prednisone or budesonide, are often used in Crohn’s disease and Ulcerative colitis to reduce inflammation in the short-term. However, it is often difficult for patients to come off of steroids while keeping their disease under control. Long-term steroid use carries with it a number of complications, such as elevated blood sugars, mood swings, insomnia and, over time, low bone density and fractures. In order to maintain patient s symptom-free and off of steroids, other disease modifying agents have been introduced over the past decade.
Immunomodulators, such as Azathioprine, 6-Mercaptopurine and Methotrexate, work by inhibiting the division of white blood cells that are responsible for the uncontrolled inflammation. They work well in Crohn’s disease and allow patients to come off of steroids while maintaining disease control. Their efficacy in Ulcerative colitis, however, is less clear. Immunomodulators require frequent blood monitoring of liver function and white blood cell count.
Anti-TNFα agents (Remicade, Humira, Cimzia) have proven to be most efficacious in controlling disease symptoms and keeping patients off of steroids. TNFα is a chemical produced by activated white blood cells in the intestine of patients with IBD. TNFα triggers a cascade of inflammatory reactions that propagate the inflammatory response. Anti-TNFα drugs are chemically engineered antibodies that allow us to attack the root of the inflammatory process and reduce inflammation. The available anti-TNFα agents are given either as an intravenous infusion every other month or as injections under the skin every other week. Although these agents work exceptionally well in both, Crohn’s disease and Ulcerative colitis, a large proportion of patients may achieve disease control without resorting to these medications. The challenge is to identify patients who require anti-TNFα agents.
New Biologic Therapies
Natalizumab (Tysabri) has been approved for use in Crohn’s disease patients who have failed anti-TNFα agents. This drug blocks the movement of white blood cells into the gut, thereby stalling inflammation. In addition to blocking the movement of white blood cells into the gut, it also blocks the movement of white blood cells into the brain and reduces the body’s ability to keep inflammation in the brain under control. This medication has caused reactivation of a virus, JC virus, which affects the brain. Therefore, all patients considered for Natalizumab therapy need to be tested for exposure to JC virus by a blood test prior to starting therapy.
Vedolizumab. This medication selectively blocks the movement of disease-causing T cells into the gut, thereby reducing inflammation. It does not affect white blood cells in the brain and, therefore, carries no risk of JC virus reactivation. Recent data has shown that Vedolizumab is effective in Ulcerative colitis patients with moderate to severe inflammation. It holds great promise for the treatment of Ulcerative colitis.
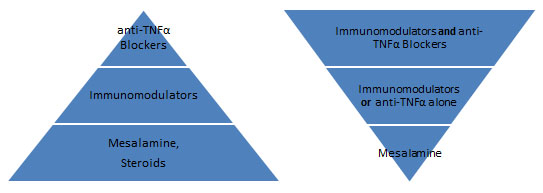
The traditional approach to therapy (diagram below) has been to start slow and escalate to stronger medications as needed if inflammation does not respond to weaker agents. However, more recent evidence suggests that a more aggressive approach allows for better disease control and fewer complications down the road. Ultimately, the choice of therapy is very individual and is based on a variety of considerations, patient preferences and on in-depth patient-doctor discussions.
To learn more about IBD medication options or to schedule an appointment with one of our doctors, contact us today.